Introduction
The prescriber ecosystem has always existed. Physicians have never made treatment decisions in isolation. What has changed is the degree to which that ecosystem now determines outcomes.
Healthcare systems today are operating under sustained pressure. Ageing populations, rising patient volumes, increasing chronic disease burden, workforce shortages, and administrative complexity have compressed the time and cognitive capacity available to prescribers. As a result, decision-making has become more distributed. Influence that once sat implicitly around the prescriber is now actively exercised across nurses, pharmacists, formulary bodies, payers, and digital systems.
These dynamics are not new. But they are now more visible, more structured, and more consequential. In many therapeutic areas, how well the ecosystem functions under load matters as much as clinical preference itself. For pharmaceutical commercial teams, this means success is increasingly determined not by engaging a single decision-maker, but by understanding and orchestrating the full network that shapes prescribing behaviour.
One of the five critical functional capabilities required for successful launches is the ability to “connect the dots”: using advanced research techniques to understand multi-stakeholder journeys and building a cross-functional view of how decisions actually happen. In an environment defined by complexity rather than novelty, commercial excellence depends on recognising the growing importance of the prescriber ecosystem.
The Reality Behind Every Prescription
In modern clinical practice, prescriptions are rarely the product of a single decision. Treatment choices are shaped through collaboration, institutional processes, and system constraints.
Research across hospital and specialty settings shows that prescribing decisions typically involve multiple non-prescribing influencers. In oncology, cardiology, diabetes, and other chronic disease areas, multidisciplinary teams play a central role in therapy selection, sequencing, and continuation.
Consider the following contributors:
- Nurses influence therapy initiation and persistence, particularly in chronic care programmes, vaccination drives, and patient education.
- Pharmacists exercise substitution authority, guide dosage decisions, and monitor adherence, directly affecting which product reaches the patient.
- Formulary committees and payers establish access boundaries through reimbursement and coverage decisions.
- Patient advocacy groups shape awareness, expectations, and demand, especially in specialty and rare diseases.
- Electronic medical record (EMR) systems nudge behaviour through alerts, defaults, and protocol-driven pathways.
Individually, each influence may appear incremental. Collectively, they form a system that determines how therapies are adopted, sustained, or deprioritised. This interconnected network is the prescriber ecosystem not a new construct, but one whose influence has intensified as healthcare complexity has increased.
Where Traditional Commercial Models Fall Short
Despite this reality, many commercial models remain anchored in prescriber-centric logic. Targeting, segmentation, and call planning often focus on individual physicians, using historical prescription data as the primary indicator of influence.
This creates a strategic blind spot.
By concentrating on the visible prescriber while overlooking the surrounding system, organisations risk misallocating resources. High-prescribing physicians may be constrained by formulary access. Nurses or pharmacists may be driving protocol adherence. Institutional guidelines may override individual preference entirely.
As healthcare delivery becomes more institutionalised, influence is no longer linear. Treating prescribing as an individual behaviour rather than a system outcome limits a company’s ability to anticipate barriers, shape adoption, or sustain momentum post launch.
From Prescriber-Centric to Ecosystem-Centric Thinking
The shift required is not a change in belief, but a change in emphasis.
Traditional commercial strategies asked:
Who writes the prescription?
Today, the more relevant question is:
Who shapes the prescription?
Ecosystem-centric thinking recognises that decisions emerge from networks, not individuals. It reflects how authority, information, and operational constraints interact across the care pathway. This perspective allows organisations to see beyond surface-level prescribing patterns and understand the real drivers of behaviour.
Prescriber Ecosystem Mapping provides the structure to do this systematically.
What Is Prescriber Ecosystem Mapping?
Defining Prescriber Ecosystem Mapping
Prescriber Ecosystem Mapping is the process of identifying, analysing, and prioritising all stakeholders, clinical, institutional, and digital that influence prescribing behaviour.
Unlike traditional segmentation, which focuses primarily on physicians’ past prescription volumes, ecosystem mapping captures the broader influence web surrounding them. It reveals how decisions are initiated, validated, constrained, or reinforced across the system.
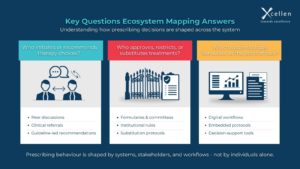
In practical terms, ecosystem mapping answers questions such as:
- Who initiates or recommends therapy choices?
- Who approves, restricts, or substitutes treatments?
- Which institutional processes and digital systems shape behaviour at the point of care?
The objective is not insight for its own sake, but to inform engagement strategies that reflect how decisions actually occur in real-world settings.
From Linear Models to Networked Systems
Pharma’s legacy engagement model is largely linear: one representative, one message, one prescriber.
Healthcare delivery, however, operates as a networked system. Decisions are influenced by institutional policy, multidisciplinary collaboration, and digital infrastructure.
A 2024 Deloitte Life Sciences Outlook highlighted that the majority of new therapy adoptions now depend on coordinated engagement across multiple stakeholders, particularly in specialty and chronic disease areas. Nurses, pharmacists, payers, and software platforms increasingly shape how and when therapies are used.
Prescriber Ecosystem Mapping makes this complexity visible. It allows organisations to trace influence pathways such as:
- A nurse identifying adherence challenges and recommending a therapy change
- A pharmacist validating brand or dosage options
- A formulary committee approving access
- An EMR prompt reinforcing the decision at the point of prescribing
Each node either accelerates or restricts adoption. Understanding these connections enables more precise resource allocation and more resilient launch strategies.
Example: Diabetes Care as a Distributed Decision System
Diabetes management illustrates how prescribing authority is shared across the ecosystem.
While physicians retain formal prescribing responsibility:
- Certified diabetes educators often influence therapy initiation and patient education
- Pharmacists monitor adherence and advise on substitutions
- Payers and formularies define access conditions and step-therapy requirements
In one example cited by McKinsey, a first-time drug launcher analysed real-world claims data and found that a small subset of healthcare professionals accounted for a disproportionate share of prescriptions for a new therapy. By focusing engagement on these high-impact nodes rather than broad physician coverage, the company reduced its launch plan budget by nearly 30% while improving performance.
This outcome was not driven by discovering new stakeholders, but by recognising where influence already concentrated within the ecosystem.
Conclusion: Seeing What Has Always Been There: More Clearly
In modern healthcare, prescriptions are shaped by systems, people, and technology working together. This has always been true. What has changed is how much those interactions now determine outcomes.
Prescriber Ecosystem Mapping brings structure to this reality. It enables organisations to move beyond prescriber-only thinking and align around how decisions truly happen. By shifting focus from individual targeting to ecosystem orchestration, life sciences companies can build strategies that are better suited to today’s healthcare environment and more resilient to the pressures shaping tomorrow’s.